Ovarian Cancer
Ovarian Cancer and its Global Impacts
Anvita Das, Dr. Lopamudra Das Roy
Published 2021
@BreastCancerHub, All Rights Reserved
Abstract
Cancer is the unregulated growth and proliferation of cells which can result from numerous causes. Ovarian cancer is cancer that affects one or both the ovaries in biological females. There are several types of ovarian cancer; epithelial, germcell, and sex-cord stromal. These can further be broken down into subcategories. Early detection is key in treating ovarian cancer, but as of right now there are no completely reliable methods to detect ovarian cancer. However, there are preventative measures and lifestyle changes that one can make to reduce their risk factor for this cancer. This paper aims to inform on the topic of ovarian cancer, and its global impact using data sourced by various cancer research institutes and organizations as well as the NIH database.
Introduction
Categories of Ovarian Cancer and other Specifications
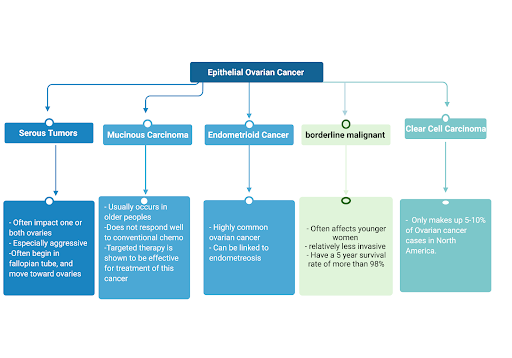
The ovaries are the female reproductive gland that produces eggs as well as the hormones estrogen and progesterone that serve many key functions including, regulation of the menstrual cycle, protecting bone health, and playing an important role in reproduction [1]. There are three types of cells that make up the ovaries and that are involved in Ovarian cancer and those are epithelial cells, germ cell, and stromal cells [2]. The three types of Ovarian Cancer are epithelial, germ cell and stromal cells based on which cell is having an overgrowth. Epithelial ovarian cancer has further been subdivided into serous carcinomas, clear cell carcinomas, mucinous carcinomas, and endometrioid carcinomas [3]. There are also non-epithelial ovarian cancers which are presented in figure [4]. These tumors are characterized by their unique molecular signaling pathways and behaviors. Another important classification is the grade of tumor which is based on how closely the cells resemble cells from healthy tissue. Grade 1 tumors are made up of cells that most look like healthy tissue and grade 3 tumor cells least resemble healthy tissue [3]. Cancers are also assigned a stage upon diagnosis based on how far the cancer has spread (Figure 2). The combination of stage, grade, and type of cancer determines how it will be treated.
Figure 2: Stages of ovarian cancer
Figure 3: Epithelial Ovarian Cancer and its subtypes [2,4-6]
Figure 4: Non-Epithelial Ovarian Cancer and its subtypes [2,7]
Risk Factors
There are hereditary, environmental, and lifestyle decisions that can increase an individual's risk for developing ovarian cancer. These can also affect the type of ovarian cancer that an individual is impacted by.
Family History
HBOC (Hereditary breast and ovarian cancer syndrome) is caused by a mutation in the BRCA1 or BRCA2 genes that are inheritable. The BRCA mutations are linked to higher probability of developing breast cancer, but they also put people at higher risk of developing ovarian cancer, fallopian tube and primary peritoneal cancer among others. These mutations are responsible for a majority of ovarian cancers. The lifetime ovarian cancer risk for women with the BRCA1 mutation ranges from 35% to 70% while, the ovarian cancer risk up to the age of 70 for women with the BRCA2 mutation ranges from 10% to 30% [2]. HNPCC (Hereditary Nonpolyposis colon cancer syndrome) is caused by several genes including MLH1, MSH2 which put individuals at a high risk for colon cancer and also leads to a 10% lifetime risk of ovarian cancer [2]. There is also a fairly new type of mutation being researched now, HRD (Homologous recombination deficiency) it has also been referred to as ‘BRCA-ness’, its most well known cause is a germline mutation in the BRCA-1 and BRCA-2 genes, but there are also somatic mutations that can cause it [8]. HR (homologous recombination) repairs DNA, so when this stops repairing DNA it is referred to as HRD. While HRD can induce apoptosis, unrepaired DNA can cause more mutations and cell proliferation [8]. Certain treatments work well for those affected by HRD such as platinum based therapies. The growing attention to HRD has brought into question the requirements for genetic testing, in the past genetic testing has been limited to those that have several blood relatives that are affected by ovarian or breast cancer, but the existence of a possibly acquired mutation like HRD has opened up the criteria for who can get genetic testing [9].
Age
Age is commonly referenced as being implicated in diagnosis and survival for ovarian cancer, however when looking at world wide peak incidence and mortality data by age varies from country to country. This may be because of increased exposure to risk factors from country to country. Age specific incidence rates for the UK have a peak for 75-79 years old, while in the Jiangsu province of china age specific incidence rates peak at 65-69 years old [9]. But in America, the peak incidence for germ cell tumors is at the ages of 15-19 [20]..
Demographics
Location plays a part in how likely a woman is to get ovarian cancer, it is shown that ovarian cancer has a higher incidence rate in developed countries particularly in urban areas. A study by researchers in China agreed with this finding where the rate of incidence in China’s urban areas was significantly higher than that of rural areas [10].
Surgical Birth Control
Forms of surgical birth control such as fallopian tube litigation have been shown to decrease the risk of epithelial ovarian cancer. It is still unclear if it can reduce the risk of all epithelial ovarian cancers or only specific subtypes [11]. A salpingectomy which is a fallopian tube removal has been shown to decrease the risk of cancer by 60% [11]. Surgical birth control is recommended to women who are at risk of ovarian cancer, and do not wish to have kids or have undergone childbirth [2,9].
Smoking
Smoking increases the risk of mucinous ovarian cancer and in current smokers risk increases by about 80%, especially for tumors of borderline malignancy [12].
Physical Activity
A lack of physical activity is linked to a 30% higher risk of ovarian cancer [13]. Various studies have also been conducted on the relationship between food and likelihood for ovarian cancer but there have been no strong linkages and more research needs to be done in this area [2].
Screening
As of right now there are not any regularly administered methods to specifically screen for ovarian cancer, and though it is under research, this lack of reliable method for screening results in a higher importance in recognizing the signs and symptoms of ovarian cancer.
TVUS- Transvaginal Ultrasound
This test uses sound waves to look at masses in the ovaries, while it can find a tumorous mass, it cannot differentiate whether the mass is a tumor or not14. Often, the masses that TVUS finds are not tumors. It also cannot differentiate between malignant and benign masses making it inefficient [14].
CA-125 blood test
Women with ovarian cancer often have high levels of a protein called CA-125 in their blood, the CA-125 blood test, tests for this protein. The problem with this test is that high levels of CA-125 are not specific to ovarian cancer but also comes up in patients with endometriosis or pelvic inflammatory disease. In addition, not all women with ovarian cancer have high levels of CA-125 making the test as a whole unreliable [14].
Self Exam
Due to the lack of regular testing for ovarian cancer it is important that people know the indicators for ovarian cancer. Some signs and symptoms are irregularities in the menstrual cycle, unexplained weight change, and abdominal swelling [15]. refer to the BCH Ovarian Cancer self exam card (figure 4).
Figure 4: BCH Ovarian Cancer Screening Card [15]
LQBTQ+
Several factors affect an individual likelihood of developing ovarian cancer, ranging from age to biological factors such as ethnicity and genotype. Note that this research only reflects the demographics of America, and subsequently their likelihood of cancer. It does not reflect the frequency of ovarian cancer among the LBTQ+ global population. Lesbian women as a group have been shown to have a higher BMI than heterosexual women which is a risk factor for ovarian cancer [16]. Ovarian cancer also disproportionately affect transgender men (biological women that have transitioned to being a man). A possible explanation for this is that trans men do not regularly get a gynecological exam as compared to cis women (biological women that identify as women) for fear of revealing their biological identity, and this infrequency in medical check ups potentially decreases the chance of the tumor being diagnosed [17].
Ovarian Cancer in America Statistics
According to the 2018 study of Ovarian cancer done by the American Cancer Society, the average risk for developing Ovarian cancer in an individual’s entire lifetime is 1.35%. They also found that the highest incidence rates for ovarian cancer are in Non-Hispanic white peoples, and the lowest rates of incidence are in Black and Asian/Pacific Islanders2. However, Black people have the second highest mortality rate when looking at racial groups which could be linked to the later stage at which cancer is discovered and treated [18,19]. Age distribution varies depending on the type of ovarian cancer, incidence peaks at the age of 70 for epithelial tumors. Whereas, for germ cell tumors the incidence peak is at the ages of 15-19 which is much younger [20]. It is important to recognize that both older and younger people must be aware of the signs and symptoms of Ovarian cancer because though it is more likely for an older person to get it, it can also affect youth. It is predicted that in this year, 2021, there will be 21,410 people that will receive a new diagnosis of ovarian cancer and that 13,770 women will die from ovarian cancer21. As of right now Ovarian cancer takes more lives than any other cancer of the female reproductive system, proving itself to be a pressing issue that we will continue to struggle with in the coming years [21].
Global Scenario
The presence of ovarian cancer is a pressing issue worldwide, it is a disease that is often caught in the late stages due to the absence of regular screening. Worldwide, the highest incidence rates of ovarian cancer are in white non hispanic peoples, followed by Hispanic, Asian and African peoples [22]. In America, though African American women have some of the lowest rates of ovarian cancer incidence, they have a higher mortality rate than non-hispanic white women which make up the majority of ovarian cancer incidences in America [21]. Additionally, tumors in African American women are caught at a more advanced stage than that of non-hispanic white women, and the median survival for African American is almost 1 year less than that of caucasian women with a p value of less than 0.0001, this is a significant decrease in lifespan [23]. Worldwide, 2020 GLOBOCAN data shows that countries with higher HDI (human development index) have a higher rate of ovarian cancer incidence than those with a medium or low HDI, an increase of 1.3 per 100,000 women. However, the data shows that there is a higher rate of mortality by ovarian cancer in lower and medium HDI countries [24]. This data has been standardized by age, however data that is not standardized by age reflects the same trend in incidence for example, Europe has a high HDI and an incidence rate of 11 per 100,000, while Africa with a lower HDI has an incidence rate of 3 per 100,00022. It can be argued that there is a lower incidence rate among countries with lower HDI because ovarian cancer occurs more frequently in older peoples, and populations in countries with a low HDI have a lower life expectancy. However, other factors such as income play an important role in mortality and incidence rates as well, middle and low-income countries often do not have adequate and accessible cancer treatment for its citizens. Greater than 90% of high income countries reported that cancer treatment services were available while only 30% of low income countries reported the same, inaccessible treatment plays a role in why 70% of ovarian cancer deaths are from low and middle income countries [25]. The M/I (mortality to incidence) ratios in developing countries are also different. It is shown that countries with a higher HDI have a lower M/I ratio meaning that there is a higher survival rate for ovarian cancer in those countries. This can be attributed to the lack of accessible treatment in low HDI countries.
In addition, many low and middle income countries do not collect sufficient data on their cancer patients, so that data that we have is limited, and it is hard to make policy changes in those countries to make cancer treatment more accessible because there is no data showing how many people are in need of treatment and thus, it is not made a priority issue. There is also stigma around ovarian cancer, it is not seen as a physical disease but rather as a spiritual misfortune and therefore patients are directed to shaman and alternative routes of medicine [9]. Availability to treatment is also a barrier in increasing the survival rates for ovarian cancer, the health expenses to treat cancer are often not affordable for a country's citizens and some countries simply do not have the treatment required, in 2020, 22% of African countries did not have access to anticancer therapies [30]. Lastly, there is a phenomenon referred to as ‘brain drain’ where skilled medical professionals and medical teachers in Africa often leave to higher HDI countries due to the availability of better jobs and salaries [31]. This creates a lack of medical professionals in Africa which contributes to the first problem mentioned, the scarcity of pathologists, it is a destructive positive feedback loop.
Predictions for 2040
Figure 6: Estimated number of new ovarian cancer cases from 2020 to 2040 in relation to countries HDI, data taken from globocan [24].
The predictions for globocan ovarian cancer show that countries with a low HDI will continue to rise in cancer cases and almost double, the same steep rise in cases is seen in medium HDI countries as well. High HDI and very high HDI countries do not have as large a percentage increase in cases when compared to low and medium HDI countries but there is still an increase. This means that ovarian cancer will continue to be a pressing issue going forward especially for low and medium HDI countries where there is a large percentage increase in ovarian cancer cases.
Conclusion
Ovarian Cancer is an issue world wide, and as shown by the projected case counts both in the US and world wide, it will continue to be a pressing issue and the burden of Ovarian cancer will continue to fall heavily on developed and developing countries. Many developed countries still do not have the access to even basic cancer medicine the WHO deems essential, meaning that more lives will be taken by ovarian cancer. Research needs to be done on how to regularly and reliably screen for ovarian cancer, so that cases are caught earlier and they have a better prognosis. In addition, it is essential that developing countries get the resources that they need to treat people living there, and to lessen the health disparities between those in lower financial brackets to those in higher ones. It is also important to not forget to include minority groups such as transgender men that are also at risk for ovarian cancer.
Materials and Methods
For this study, data was sourced from the NIH, and from other sources listed in the citations that specialize in cancer research.
References
https://www.cancercenter.com/cancer-types/ovarian-cancer/types
Catherine A. Shu et al. (2015) Ovarian Clear Cell Carcinoma, Outcomes by Stage: The MSK Experience. Gynecol Oncol. 139: 236–241.
Jonathan S. Berek, et al. (2003) Nonepithelial Ovarian Cancer. Holland-Frei Cancer Medicine. 6th edition.
Renata Rodrigues da Cunha Colombo Bonadio et al. (2018) Homologous recombination deficiency in ovarian cancer: a review of its epidemiology and management. Clinics (Sao Paulo). 2018; 73
Bing Wang, et al. (2014) Time trends of ovarian cancer incidence in China. Asian Pac J Cancer. 15,191-3.
Falconer H, Yin L, Gronberg H, Altman D. Ovarian cancer risk after salpingectomy: a nationwide population-based study. J Natl Cancer Inst. 2015;107.
Collaborative Group on Epidemiological Studies of Ovarian Cancer, Beral V, Gaitskell K, et al. Ovarian cancer and smoking: individual participant meta-analysis including 28,114 women with ovarian cancer from 51 epidemiological studies. Lancet Oncol. 2012;13: 946-956.
Cannioto R, LaMonte MJ, Risch HA, et al. Chronic recreational physical inactivity and epithelial ovarian cancer risk: evidence from the Ovarian Cancer Association Consortium. Cancer Epidemiol Biomarkers Prev. 2016;25: 1114-1124.
https://www.breastcancerhub.org/educational-cards/ovarian-cancer
Long B, Chang J, Ziogas A, Tewari KS, Anton-Culver H, Bristow RE. Impact of race, socioeconomic status, and the health care system on the treatment of advanced-stage ovarian cancer in California. Am J Obstet Gynecol. 2015;212: 468 e461-469.
Bristow RE, Powell MA, Al-Hammadi N, et al. Disparities in ovarian cancer care quality and survival according to race and socioeconomic status. J Natl Cancer Inst. 2013;105: 823-832.
SEER*Stat Database: NAACCR Incidence Data – CiNA Analytic File, 1995-2014, for Expanded Races, Custom File With County, ACS Facts and Figures projection Project (which includes data from CDC’s National Program of Cancer Registries (NPCR), CCCR’s Provincial and Territorial Registries, and the NCI’s Surveillance, Epidemiology and End Results (SEER) Registries), certified by the North American Association of Central Cancer Registries (NAACCR) as meeting high-quality incidence data standards for the specified time periods, submitted December 2016.
https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html
Chornokur, Ganna et al. “Global ovarian cancer health disparities.” Gynecologic oncology vol. 129,1 (2013): 258-64. doi:10.1016/j.ygyno.2012.12.016
Barnholtz-Sloan, et al. Ethnic differences in survival among women with ovarian carcinoma. Cancer, 94: 1886-1893.
Sung, H, Ferlay et al. (2020) GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021: 71: 209- 249.
Eniu A, Cherny NI, Bertram M, et al. (2019) Cancer medicines in Asia and Asia-Pacific: What is available, and is it effective enough?. ESMO Open. 2019:4
http://hdr.undp.org/sites/default/files/Country-Profiles/USA.pdf
http://hdr.undp.org/sites/all/themes/hdr_theme/country-notes/NGA.pdf
http://hdr.undp.org/sites/all/themes/hdr_theme/country-notes/UGA.pdf
Adel-Whahab, May et al (2013) Status of radiotherapy resources in Africa: an International Atomic Energy Agency analysis, The Lancet Oncology, Vol 14 Issue 4: 168-175
Vanderpuye V, Hammad N, et al. (2019) Cancer care workforce in Africa: perspectives from a global survey. Infect Agent Cancer;14:11.